Dr. Trudy Simmons, Milton Counseling & Coaching, on Trauma Recovery, Faith-Based Counseling, Anxiety, Depression, Relationship Restoration, and Ironman Discipline (North Fulton Business Radio, Episode 927)
On this episode of North Fulton Business Radio, host John Ray welcomes Dr. Trudy Simmons, founder of Milton Counseling & Coaching. Dr. Trudy is a counselor, author, speaker, and Ironman world champion athlete who brings a holistic approach to mental and emotional wellness. With a doctorate in counseling and 20 years of experience, she specializes in trauma recovery, emotional regulation, and relationship restoration, blending evidence-based therapeutic practices with biblical truth.
Hearing clients’ stories of defeat and feeling stuck inspired Dr. Trudy to transition from personal trainer to counselor. She explains the difference between counseling (which addresses past trauma) and coaching (which propels clients forward into action). Drawing on her completion of 16 Ironman races, including the Kona World Championship, and a 100-mile race in honor of her late father, she discusses how endurance sports demonstrate that hard things are possible and mirror the discipline needed for life transformation. Dr. Trudy describes her practice serving clients from age 16 to 80, helping them address anxiety, hopelessness, relationship struggles, and feeling stuck in their personal or professional lives.
John Ray is the host of North Fulton Business Radio. The show is produced by John Ray and North Fulton Business Radio, LLC, an affiliate of Business RadioX®, and is recorded inside Renasant Bank in Alpharetta.
Key Takeaways from This Episode
- Dr. Trudy transitioned from 20 years as a personal trainer to counseling after recognizing she could help people get unstuck not just physically, but mentally, emotionally, and spiritually.
- Counseling addresses past trauma and helps pull clients out of difficult experiences, while coaching focuses on moving forward and taking action toward future goals.
- Completing 16 Ironman races, including the Kona World Championship and a 100-mile race, demonstrates that seemingly impossible challenges are achievable with consistency, discipline, and determination.
- Common signs someone may benefit from counseling include anxiety, loneliness, hopelessness, loss of passion, relationship struggles, and feeling stuck or unable to move forward in life.
Topics Discussed in this Episode
00:20 John Ray introduces the show and guest Dr. Trudy Simmons
02:06 Dr. Trudy Simmons introduces Milton Counseling & Coaching
02:47 Dr. Trudy’s backstory and transition from personal trainer to counselor
03:47 Completing 16 Ironman races and the Kona World Championship
04:38 How endurance sports discipline informs her counseling practice
06:02 The difference between counseling and coaching
08:17 Dr. Trudy’s holistic approach to body, mind, and spirit
11:42 Faith-based counseling and integrating biblical truth with therapy
14:08 Working with emotions and creating safe space for clients
19:24 Signs that indicate someone should seek counseling
20:17 What happens in the first counseling session
21:00 Success stories from Dr. Trudy’s practice
22:39 How to connect with Milton Counseling & Coaching
Dr. Trudy Simmons, PhD
Dr. Trudy Simmons, PhD, is a highly respected counselor, author, speaker, Ironman world champion athlete, and the host and producer of the award-winning Christian talk show The Christian View. As the founder of Milton Counseling and Coaching and The Christian View Media, Inc., she is dedicated to equipping individuals, families, and communities with the tools to live healed, purposeful, and wholehearted lives.
With a doctorate in counseling and decades of clinical experience, Dr. Trudy is known for her compassionate, practical, and faith-centered approach to mental and emotional wellness. She specializes in trauma recovery, emotional regulation, relationship restoration, and mind-body-spirit wholeness. Her work blends evidence-based therapeutic practices with biblical truth, empowering others to break cycles, renew their minds, and step boldly into their God-given purpose.
A fierce endurance athlete, Dr. Trudy has completed 16 Ironman races, competed in the Ironman World Championship in Kona, and finished multiple ultra-distance races—including a 100-mile run. She draws on these transformative athletic experiences to teach principles of perseverance, resilience, and identity, helping others push past limitations and embrace a lifestyle of purpose, discipline, and victory.
Dr. Trudy is a sought-after speaker for women’s events, corporate trainings, leadership retreats, churches, and podcasts. She teaches on topics such as purpose, emotional healing, spiritual formation, overcoming limiting beliefs, leadership development, and becoming “Fit for Purpose” in body, mind, and spirit. Her upcoming book, Fit for Purpose, weaves her personal journey, Ironman discipline, biblical wisdom, and counseling insights into a compelling guide for whole-life transformation.
As a wife, mother of two, and influential voice in Christian media, Dr. Trudy is deeply committed to helping people rewrite their stories, deepen their faith, and live with courage, clarity, and joy. Whether through counseling, coaching, television, writing, or endurance sports, her mission remains the same: to help people heal, grow, and live out the purpose for which they were created.
Milton Counseling & Coaching
Milton Counseling & Coaching, founded and led by Dr. Trudy Simmons, PhD, is a premier mental and emotional wellness practice dedicated to helping individuals, couples, and families heal, grow, and thrive. Rooted in evidence-based therapeutic practices and a compassionate, faith-informed approach, the practice specializes in trauma recovery, emotional and relational health, anxiety, depression, and whole-person transformation.
With a focus on creating a safe, confidential, and supportive environment, Milton Counseling & Coaching empowers clients to navigate life transitions, rewrite unhealthy patterns, strengthen relationships, and discover renewed purpose and clarity. Through counseling, coaching, workshops, and customized growth plans, the practice equips clients with practical tools to build resilience, cultivate emotional intelligence, and experience long-term change—body, mind, and spirit.
Milton Counseling & Coaching has become known for its warm professionalism, client-centered care, and firm dedication to helping people live emotionally healthy, purpose-driven lives.
Renasant Bank supports North Fulton Business Radio
 Renasant Bank has humble roots, having started in 1904 as a $100,000 bank located in a Lee County, Mississippi, bakery. Since then, Renasant has grown into one of the Southeast’s strongest financial institutions, boasting over $26 billion in assets and more than 280 offices offering banking, lending, wealth management, and financial services throughout the region. All of Renasant’s success stems from the commitment of each banker to invest in the communities they serve, which in turn helps them better understand the people they serve. At Renasant Bank, their banking professionals understand you because they work and live alongside you every day.
Renasant Bank has humble roots, having started in 1904 as a $100,000 bank located in a Lee County, Mississippi, bakery. Since then, Renasant has grown into one of the Southeast’s strongest financial institutions, boasting over $26 billion in assets and more than 280 offices offering banking, lending, wealth management, and financial services throughout the region. All of Renasant’s success stems from the commitment of each banker to invest in the communities they serve, which in turn helps them better understand the people they serve. At Renasant Bank, their banking professionals understand you because they work and live alongside you every day.
Website | LinkedIn | Facebook | Instagram | X (Twitter) | YouTube
Beyond Computer Solutions supports North Fulton Business Radio
Whether you’re a law firm, medical practice, or manufacturer, there’s one headline you don’t want to make: “Local Business Pays Thousands in Ransom After Cyberattack.” That’s where Beyond Computer Solutions comes in. They help organizations like yours stay out of the news and in business with managed IT and cybersecurity services designed for industries where compliance and reputation matter most.
Whether they serve as your complete IT department or simply support your internal team, they are well-versed in HIPAA, secure document access, written security policies, and other essential aspects that ensure your safety and well-being. Best of all, it starts with a complimentary security assessment.
Website | LinkedIn | Facebook | YouTube
About North Fulton Business Radio and host John Ray
With over 900 episodes and having featured over 1,400 guests, North Fulton Business Radio is the longest-running podcast in the North Fulton area, covering business in our community like no one else. We are the undisputed “Voice of Business” in North Fulton!
The show invites a diverse range of business, non-profit, and community leaders to share their significant contributions to their respective markets, communities, and professions. There is no discrimination based on company size, and there is never any “pay to play.” North Fulton Business Radio supports and celebrates businesses by sharing positive stories that traditional media ignore. Some media lean left. Some media lean right. We lean business.

John Ray is the host of North Fulton Business Radio. John and the team at North Fulton Business Radio, LLC, an affiliate of Business RadioX®, produce the show, which is recorded inside Renasant Bank in Alpharetta.
The studio is located at 275 South Main Street, Alpharetta, GA 30009.
You can find the entire archive of shows by following this link. The show is accessible on all major podcast apps, such as Apple Podcasts, Spotify, Google, Amazon, iHeart Radio, and many others.
 John Ray also operates his own business advisory practice. John’s services include advising solopreneurs and small professional services firms on their value, their positioning and business development, and their pricing. His clients are professionals who are selling their expertise, such as consultants, coaches, attorneys, CPAs, accountants, bookkeepers, marketing professionals, and other professional services practitioners.
John Ray also operates his own business advisory practice. John’s services include advising solopreneurs and small professional services firms on their value, their positioning and business development, and their pricing. His clients are professionals who are selling their expertise, such as consultants, coaches, attorneys, CPAs, accountants, bookkeepers, marketing professionals, and other professional services practitioners.
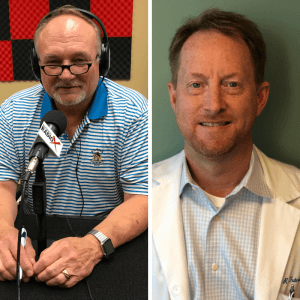
John is the author of the five-star rated book The Generosity Mindset: A Journey to Business Success by Raising Your Confidence, Value, and Prices, praised by readers for its practical insights on raising confidence, value, and prices.






 As numbers 13 and 14 of 14 siblings and the mothers of seven children and six children, Kay Bodude and Myrrie Hayes never imagined one day they would own and operate a multimillion-dollar company.
As numbers 13 and 14 of 14 siblings and the mothers of seven children and six children, Kay Bodude and Myrrie Hayes never imagined one day they would own and operate a multimillion-dollar company. Their first “legitimate” business was a uniform store. They sold medical uniforms, medical equipment, and school uniforms.
Their first “legitimate” business was a uniform store. They sold medical uniforms, medical equipment, and school uniforms.





 Sherry Anshara is an international bestselling author, professional speaker, former radio host of “Conscious Healing”, and contributing writer to national and international publications on the subject of the Anshara Method of Accelerated Healing & Abundance and overall wellness. Sherry Anshara utilizes her experience and expertise as a Medical Intuitive as the foundation of her groundbreaking work with Cellular Memory, which she calls the Anshara Method.
Sherry Anshara is an international bestselling author, professional speaker, former radio host of “Conscious Healing”, and contributing writer to national and international publications on the subject of the Anshara Method of Accelerated Healing & Abundance and overall wellness. Sherry Anshara utilizes her experience and expertise as a Medical Intuitive as the foundation of her groundbreaking work with Cellular Memory, which she calls the Anshara Method.