Acid and Ulcers (Episode 81, To Your Health with Dr. Jim Morrow)
On this episode of To Your Health, Dr. Jim Morrow of Village Medical offered information about indigestion, ulcers, and stomach issues. He detailed the symptoms of indigestion that sometimes can overlap with other serious conditions. Dr. Morrow also talked about what causes indigestion, what can be done to treat it, the causes and treatments of peptic ulcers, and more.
To Your Health is brought to you by Village Medical (formerly Morrow Family Medicine), which brings the care back to healthcare.
About Village Medical (formerly Morrow Family Medicine)
Village Medical, formerly Morrow Family Medicine, is an award-winning, state-of-the-art family practice with offices in Cumming and Milton, Georgia. The practice combines healthcare information technology with old-fashioned care to provide the type of care that many are in search of today. Two physicians, three physician assistants and two nurse practitioners are supported by a knowledgeable and friendly staff to make your visit to Village Medical one that will remind you of the way healthcare should be. At Village Medical, we like to say we are “bringing the care back to healthcare!” The practice has been named the “Best of Forsyth” in Family Medicine in all five years of the award, is a three-time consecutive winner of the “Best of North Atlanta” by readers of Appen Media, and the 2019 winner of “Best of Life” in North Fulton County.
Village Medical offers a comprehensive suite of primary care services including preventative care, treatment for illness and injury, and management of chronic conditions such as diabetes, congestive heart failure, chronic obstructive pulmonary disease (COPD) and kidney disease. Atlanta-area patients can learn more about the practice here.
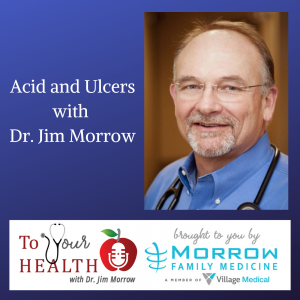
Dr. Jim Morrow, Village Medical, and Host of To Your Health with Dr. Jim Morrow
 Dr. Jim Morrow is the founder of Morrow Family Medicine. He has been a trailblazer and evangelist in healthcare information technology, was named Physician IT Leader of the Year by HIMSS, a HIMSS Davies Award Winner, the Cumming-Forsyth Chamber of Commerce Steve Bloom Award Winner as Entrepreneur of the Year and he received a Phoenix Award as Community Leader of the Year from the Metro Atlanta Chamber of Commerce. He is married to Peggie Morrow and together they founded the Forsyth BYOT Benefit, a charity in Forsyth County to support students in need of technology and devices. They have two Goldendoodles, a gaggle of grandchildren and enjoy life on and around Lake Lanier.
Dr. Jim Morrow is the founder of Morrow Family Medicine. He has been a trailblazer and evangelist in healthcare information technology, was named Physician IT Leader of the Year by HIMSS, a HIMSS Davies Award Winner, the Cumming-Forsyth Chamber of Commerce Steve Bloom Award Winner as Entrepreneur of the Year and he received a Phoenix Award as Community Leader of the Year from the Metro Atlanta Chamber of Commerce. He is married to Peggie Morrow and together they founded the Forsyth BYOT Benefit, a charity in Forsyth County to support students in need of technology and devices. They have two Goldendoodles, a gaggle of grandchildren and enjoy life on and around Lake Lanier.
The complete show archive of To Your Health with Dr. Jim Morrow addresses a wide range of health and wellness topics.
Dr. Morrow’s Show Notes
What is indigestion (dyspepsia)?
- Indigestion, also known as dyspepsia, is a common condition.
- It can happen when your body has trouble digesting food.
- It occurs in your gastrointestinal (GI) tract.
- The GI tract is a group of organs that plays a part in digestion.
- Anyone can get indigestion.
- You can get it on occasion,
- or it can be an ongoing problem.
- The symptoms and causes vary by case.
- If there is no known cause for indigestion, it is referred to as functional dyspepsia.
Symptoms of indigestion
- Indigestion can feel like a stomachache. You can have a range of symptoms including:
- Pain, discomfort, or a burning feeling in your chest or stomach
- Burping
- Bloating
- Gurgling stomach and/or gas
- Acid reflux
- Heartburn
- Nausea and/or vomiting
- Talk to your doctor if symptoms continue for more than two weeks. Seek medical care right away if your symptoms are severe, such as:
- Shortness of breath
- Trouble swallowing
- Ongoing vomiting
- Throwing up blood
- Sudden pain in the chest, arm, neck, or jaw
- Cold sweats
- Thick, black, or bloody stool
What causes indigestion?
- A lot of factors can cause indigestion. These include:
- Eating certain foods, such as those that are spicy and fatty, and those with lots of acid or fiber
- Eating too late in the day
- Drinking alcohol or too much caffeine
- Taking certain medicines
- Smoking
- Not sleeping
- Problems in your GI tract or other health issues also can cause indigestion. These include:
- Acid reflux or gastroesophageal reflux disease (GERD):
- This is when your food and drink come back up from your stomach after eating or drinking.
- It’s in the form of acid and can come into your esophagus, the tube-like organ connecting your mouth and stomach.
- Acid reflux also can produce vomiting.
- This condition also may cause heartburn.
- Irritable bowel syndrome:
- This disorder affects your intestines.
- Symptoms include stomach pain, bloating, gas, constipation, and diarrhea.
- Infection:
- A bacterial infection from Helicobacter pylori (H. pylori) can cause indigestion.
- Gastroparesis:
- This condition affects digestion. If muscles in your GI tract stop working, your body slows down or stops the movement of food. Symptoms include nausea, vomiting, stomach pain, bloating, and acid reflux.
- Ulcer:
- This is a sore on the lining of your stomach (peptic ulcer), small intestine, or esophagus.
- Gastritis:
- This is inflammation of your stomach lining.
- Stomach cancer:
- This is a rare condition, but indigestion can be one of its signs.
How is indigestion diagnosed?
- Your doctor will review your symptoms and perform a physical exam.
- They may order tests to determine the cause of indigestion.
- Those tests can include blood work, urine/stool tests, or an X-ray or ultrasound.
- Sometimes your doctor may perform an upper endoscopy to see inside your stomach.
- Your doctor will insert a thin tube with a camera on the end into your esophagus.
- This will be done after you’re given medicines to go to sleep.
Can indigestion be prevented or avoided?
- There are ways to prevent indigestion.
- To start, you need to know your body and how it reacts to different food and drinks.
- Spicy and acidic foods and carbonated drinks can trigger indigestion.
- Try to avoid those things when possible.
- Eat smaller meals throughout the day, and don’t eat too late at night.
- Don’t lie down too soon after eating.
- Limit the use of alcohol.
- If you use tobacco, try to quit.
- Stress and lack of sleep also can worsen symptoms.
Indigestion treatment
- Your treatment will depend on what is causing your indigestion.
- Your doctor can help you decide which treatment is best for you.
- Some over-the-counter medicines may help your symptoms.
- Check with your doctor before starting something new.
- Antacids (Tums) work against the acid in your system.
- Proton pump inhibitors
- omeprazole and
- lansoprazole
- help block the site of acid production in your stomach.
- Histamine blockers
- help reduce pain and symptoms, but should not be used long-term.
- Do not take pain and anti-inflammatory medicines
- for your symptoms.
- They do not help and can worsen your condition, especially if used often.
- If you have a stomach ulcer, you may need to take an acid-blocking medicine.
- But your ulcer can be cured.
- If you have an infection in your stomach, you also may need to take an antibiotic.
- Prevention methods for indigestion also are forms of treatment.
- These include changing your diet and the way you eat.
- Also get more sleep and reduce your level of stress.
- These include changing your diet and the way you eat.
Living with indigestion
- Most people who have indigestion lead a normal life.
- You may need to make some lifestyle changes or take medicine to treat your symptoms.
- Exercise regularly and maintain a healthy weight.
- In rare cases, indigestion can be the sign of a serious problem.
- Examples include a deep stomach ulcer or stomach cancer.
- If you have any of the following symptoms, contact your doctor right away:
- You recently lost weight without trying.
- You have trouble swallowing.
- You have severe vomiting.
- You have black, tarry bowel movements.
What is peptic ulcer disease?
- A peptic ulcer is a sore or raw area in the lining of the stomach.
- It also can occur near the top of the small intestine.
- This area of the small intestine is called the duodenum.
- The lining is damaged by the acids your body uses to digest food.
- It also can occur near the top of the small intestine.
Symptoms of peptic ulcer disease
- The most common symptom is a burning pain in your stomach.
- It usually lasts for a few minutes to a few hours.
- It comes and goes for days or weeks at a time.
- The burning typically occurs between meals and at night.
- Small ulcers may cause no symptoms.
- Other symptoms can include:
- A feeling of fullness
- Difficulty drinking as much liquid as usual
- Hunger or an empty feeling in your stomach after you eat
- Mild nausea
- Stomach pain that wakes you up at night
- Less common symptoms include:
- Bloating
- Burping
- Poor appetite
- Bloody or dark stools
- Chest pain
- Fatigue
- Weight loss
- Vomiting
- Complications include:
- Bleeding (this occurs from a broken blood vessel in the small intestine)
- Perforation (tear)
- A blockage
- Peritonitis (infection)
What causes peptic ulcer disease?
- The main cause is the bacterial infection, Helicobacter pylori (H. pylori).
- Another common cause is long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
- This includes aspirin, ibuprofen, and naproxen.
- In rare cases, the disease can be caused by cancerous and noncancerous tumors.
- A less common cause is a rare disorder called Zollinger-Ellison syndrome.
How is peptic ulcer disease diagnosed?
- Your doctor will do a physical exam.
- Your doctor may schedule a special procedure to look at your stomach.
- This is called an endoscopy.
- For this procedure, you’ll be given medicine to relax.
- The medicine may make you fall asleep.
- The doctor will insert a thin, flexible tube down your throat.
- A tiny camera on the end of the tube displays the lining of your stomach and duodenum.
- The doctor may take a sample of your stomach lining (a biopsy).
- This is done to test for H. pylori.
- Blood, breath, and stool sample testing can also be used to check for H. pylori.
Can peptic ulcer disease be prevented or avoided?
- Stress and spicy foods don’t cause ulcers.
- However, they can make them worse.
- Smoking and alcohol can cause a peptic ulcer.
- Men should limit alcohol to no more than 2 drinks per day.
- Women should have no more than 1 drink per day.
- Talk to your doctor if you take aspirin, ibuprofen, or naproxen regularly.
Peptic ulcer disease treatment
- Your doctor may begin by prescribing medicine.
- Your doctor may suggest other treatments for other causes.
- If you have H. pylori, your doctor will treat the infection with specific therapy.
- Your doctor may recommend medicines to neutralize your stomach acid.
- This will protect the lining in your stomach, too.
- These include:
- Protein pump inhibitors.
- Histamine receptor blockers.
- Cytoprotective agents. This includes sucralfate
- If NSAIDs cause your ulcer, you may need to stop or reduce the amount you take.
- You may need to switch to another type of medicine for pain.
Living with peptic ulcer disease
- Most ulcers heal within about 8 weeks.
- Peptic ulcers come and go.
- You have to do what you can to reduce your risk.
- If you smoke or chew tobacco, ask your doctor about how to quit.
- Eat a well-balanced diet.
- Avoid foods that cause discomfort.
- These include
- alcohol,
- coffee,
- caffeinated soda,
- fatty foods,
- chocolate,
- and spicy foods.
- Avoid eating late at night.
- Talk to your doctor about alternatives to NSAIDs.
- These include
- Peptic ulcers come and go.
Take all medicines with plenty of water.


 Special thanks to A&S Culinary Concepts for their support of this edition of North Fulton Business Radio. A&S Culinary Concepts, based in Johns Creek, is an award-winning culinary studio, celebrated for corporate catering, corporate team building, Big Green Egg Boot Camps, and private group events. They also provide oven-ready, cooked from scratch meals to go they call “Let Us Cook for You.” To see their menus and events, go to
Special thanks to A&S Culinary Concepts for their support of this edition of North Fulton Business Radio. A&S Culinary Concepts, based in Johns Creek, is an award-winning culinary studio, celebrated for corporate catering, corporate team building, Big Green Egg Boot Camps, and private group events. They also provide oven-ready, cooked from scratch meals to go they call “Let Us Cook for You.” To see their menus and events, go to 








 Dr. Jim Morrow is the founder and CEO of Morrow Family Medicine. He has been a trailblazer and evangelist in the area of healthcare information technology, was named Physician IT Leader of the Year by HIMSS, a HIMSS Davies Award Winner, the Cumming-Forsyth Chamber of Commerce Steve Bloom Award Winner as Entrepreneur of the Year and he received a Phoenix Award as Community Leader of the Year from the Metro Atlanta Chamber of Commerce. He is married to Peggie Morrow and together they founded the
Dr. Jim Morrow is the founder and CEO of Morrow Family Medicine. He has been a trailblazer and evangelist in the area of healthcare information technology, was named Physician IT Leader of the Year by HIMSS, a HIMSS Davies Award Winner, the Cumming-Forsyth Chamber of Commerce Steve Bloom Award Winner as Entrepreneur of the Year and he received a Phoenix Award as Community Leader of the Year from the Metro Atlanta Chamber of Commerce. He is married to Peggie Morrow and together they founded the